Media Contact

NSW Health Pathology researchers have been tracking how the COVID-19 virus mutates in a first-of-its-kind study, revealing patterns that could help predict the emergence of future variants.
In the early days of the COVID-19 pandemic, as the world scrambled to understand the fast-moving virus, a team of Australian researchers set out to study how the virus would evolve long term.
With millions of infections unfolding globally and new variants rapidly emerging, they wanted to learn how SARS-CoV‑2 — the virus that causes COVID-19 — would evolve in a controlled lab setting, and if it would weaken over time.
Fast forward more than five years and their findings, published in the Journal of Virology, have confirmed the remarkable adaptability of the virus, shedding light on common mutations which emerge repeatedly and independently in different strains.
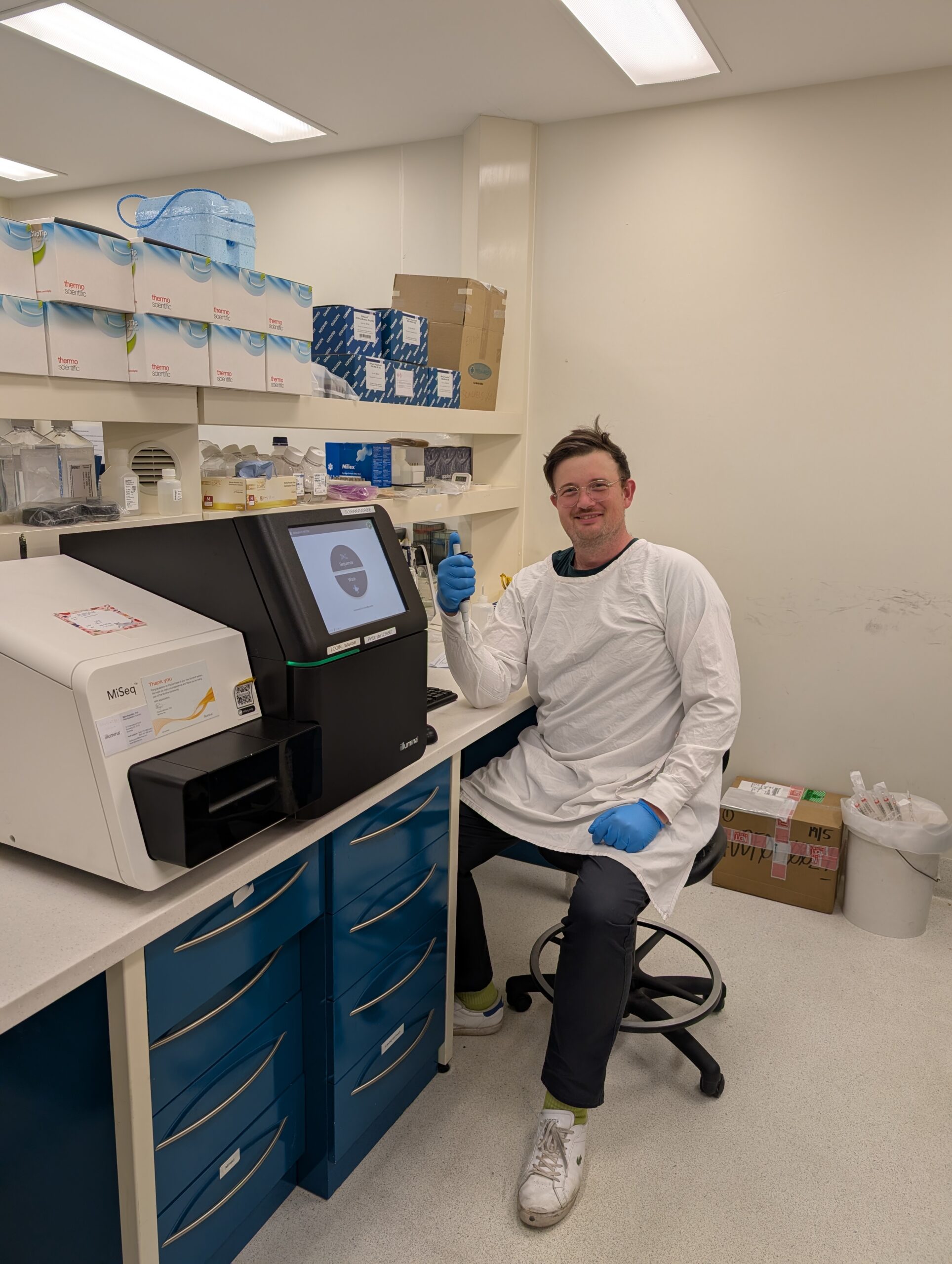
The research, which is the most extensive of its kind to date, could help predict the emergence of future variants and inform treatment and prevention design, said first author Dr Charles Foster, from NSW Health Pathology’s Virology Research Laboratory at Prince of Wales Hospital and UNSW’s School of Biomedical Sciences.
“This work could help us anticipate how the virus might evolve next. If we can identify mutations that arise repeatedly —even in a lab setting—it gives us a chance to predict which changes could emerge in the real world, so we can prepare for them,” Dr Foster said.
Tracking the virus in a controlled environment
Whole-genome sequencing of COVID-19 cases enabled global contract tracing efforts during the pandemic and the identification of mutations of concern. But further research was needed to understand how the virus evolves.
In this multi-year study researchers examined how 11 virus samples from nine different COVID-19 variants, including Alpha, Delta, and Omicron, mutated over time. The samples were grown in Vero E6 cells – monkey kidney cells commonly used in virus research which lack a strong immune response.
Using a method called serial passaging, they transferred the virus from one batch of cells to another repeatedly, between 33 to 100 times, well above the 15 passages in previously published research for SARS-CoV‑2. It’s a method often used to study viral changes, and is used in vaccine development to attenuate, or weaken, a virus in a controlled way.
“It’s challenging to understand how COVID-19 adapts only by looking at real-world cases because there are so many variables at play,” Dr Foster said.
“By growing the virus over many generations in a controlled lab environment, we can observe how it evolves without the influence of the immune system or treatments. That gives us a clearer picture of its natural evolutionary pathways.”
The passaging was conducted in a secure laboratory and did not aim to increase the transmissibility or severity of the virus samples. The use of Vero E6 cells further limited risks to human health.
How the virus evolved in the lab
The researchers tracked how the virus’s genetic code changed during passaging, specifically, how many mutations appeared and whether they stuck around or disappeared.
“One goal of this was to see if mutations would develop that mirrored what’s going on in the real world. But on the flip side, we also wanted to see if new mutations would arise that haven’t been seen yet and what impact they might have,” Dr Foster said.
The viruses continually evolved, even the sample which was put through 100 passages.
“We gave the virus optimal conditions to keep developing and wanted to see whether it would eventually attenuate—basically weaken—over time. It didn’t,” Dr Foster said.
“In all cases, by the time we stopped, the viruses were still growing happily and picking up mutations.”
There were new mutations which popped up repeatedly in different strains – a phenomenon known as convergent evolution – as well as changes which mirrored those seen in real world outbreaks.
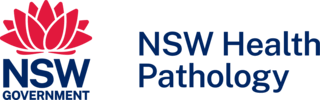
The similarities suggest the virus may be naturally inclined to develop certain changes, regardless of the environment and external pressures, said senior author Professor William Rawlinson, Director of Microbiology at Prince of Wales Hospital and Senior Medical Virologist at NSW Health Pathology.
“Some mutations which help the virus adapt may be driven by the makeup of the virus itself, rather than a bid to evade immunity,” he said.
“Some of the changes we saw in humans were also happening in vitro, which suggests it’s not just about transmissibility or immune evasion—it’s also about the structure and function of the virus itself,” Prof. Rawlinson said.
“They could develop these important mutations even in the absence of a catalyst.”
While many of the changes occurred in the spike protein—the part of the virus that helps it enter human cells—other parts of the virus also mutated, in some cases at even higher rates. Several of the mutations are already known to reduce the effectiveness of certain vaccines.
Prof. Rawlinson stressed that the research reflected how a virus might evolve in the real world, but did not speed up its evolution. He added the risk of the virus developing adverse genetic changes was lower in the controlled lab environment, than in a real-world setting where it would adapt to immune pressures.

Next steps: Sharing data and deepening understanding
Though the research stripped away the complexities of real-world transmission, it offers valuable insights that could help researchers and public health authorities better predict how the virus will evolve and inform future treatment and prevention strategies.
Dr Foster suspects the lab findings will translate to the real world, with the virus to continue adapting long term, just subject to more evolutionary pressures.
Further research will be needed, particularly on the repeat mutations, to better understand how the virus changes over time and how this compares to the real-world infection.
The sequencing data and analysis code have been made publicly available by the researchers, so it can serve as a resource for other experts.
“We’ve made all of our sequencing data freely available so other researchers can dig into it, compare it with clinical samples, and hopefully uncover even more about how this virus evolves,” Dr Foster said.
(This article was originally published by the UNSW newsroom.)