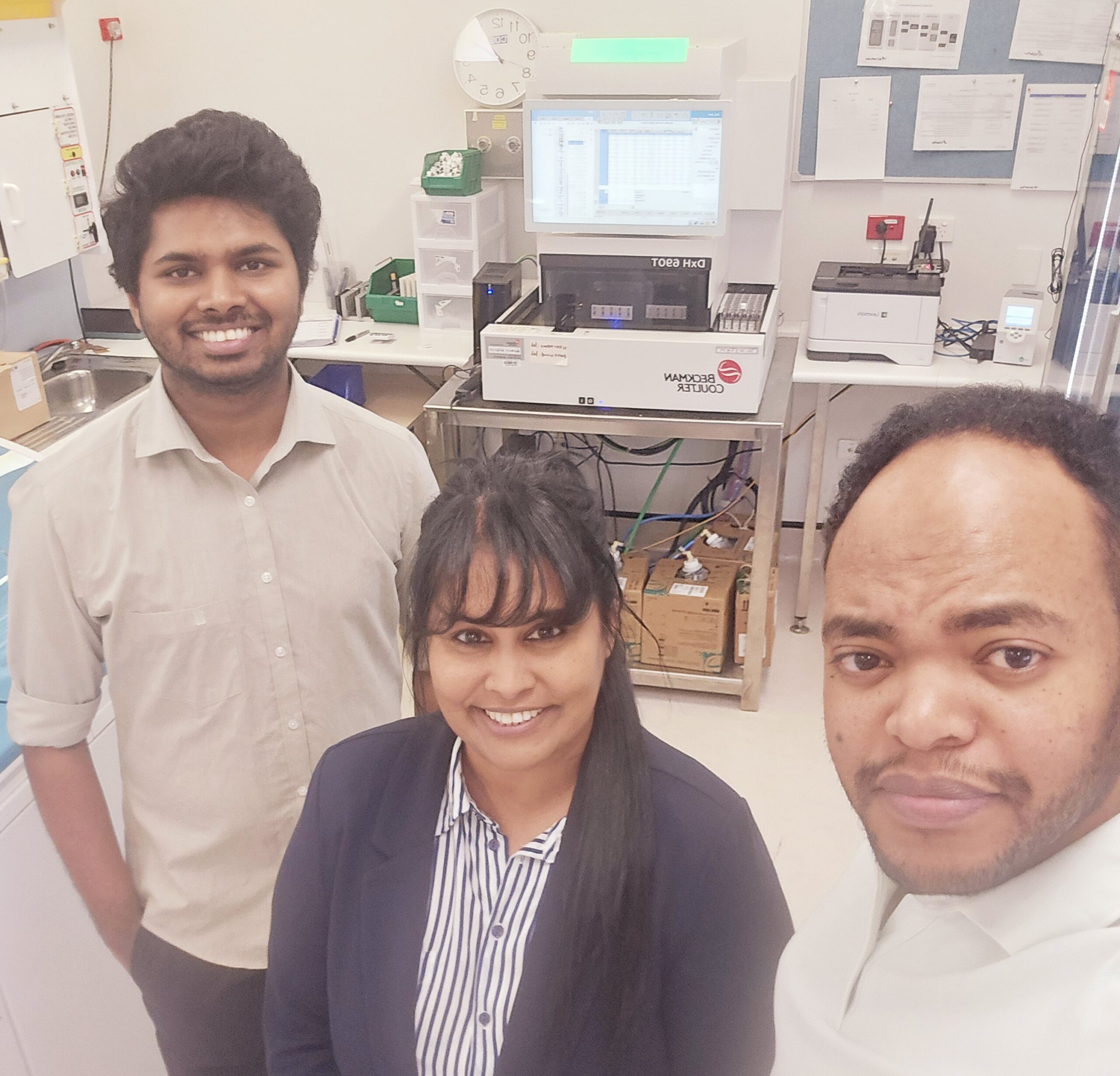
Sunita Goundar says her decision to move from Sydney to Walgett in northern NSW was about giving back to the community but has also changed her life for the better.
Sunita took up the role of Laboratory Manager at Walgett in September 2023.
“I’d been working in pathology in Sydney for almost 20 years, the last 14 with NSW Health Pathology,” Sunita explains.
“I’m from Fiji originally and when you come to a country like Australia to study and work, it gives you so many privileges, and you just want to give back because Australia has given me so much.”
Sunita loves exploring regional and rural Australia. A few years ago, on a trip to regional Queensland, she got talking to some locals about how hard it was to access healthcare and realised she wanted to help.
“I actually felt that I could do something, this was something I could do to help smaller communities.”
Does she miss living in a city the size of Sydney, where she has a network of friends and family?
“Not at all! Walgett is a beautiful place, the people are very friendly. I have colleagues who arrive every morning at 6am and we all go for a morning walk together. Everyone here is like a family, not like colleagues,” Sunita says.
“I make friends very quickly, and unlike Sydney where you don’t even know your neighbours, here, everyone knows everyone. My health has also improved. I have asthma and the air here is just so much cleaner and fresher than Sydney.
“Of course it’s very different to Sydney, but I was very clear in my thinking that I am here for a purpose, and I am happy to be here.”
Sunita admits she was afraid of one thing moving to regional NSW – snakes.
“In my first couple of months I saw a couple of eastern brown snakes. But you know what? I’m not scared anymore because if you leave them alone they don’t actually harm you.”
Sunita says she was lucky to get accommodation near the hospital, as Walgett is no different to other regional areas where rental housing is in short supply.
“I’m only one minute away from work – a very short commute! We have a gym here as well, so I have everything I need close by.”
Sunita says the Walgett laboratory has a range of services and the work is challenging.
“We’ve got a biochemistry department, a haematology department, we also do blood transfusion and recently we’ve been dealing with more complicated cases for the blood bank.
“If there is an MTP (Massive Transfusion Protocol) we are here dispensing bloods, not just locally, but also for surrounding areas.
“We have a collection centre at Lightning Ridge and we also serve Collarenabri District Hospital, the AMS (Aboriginal Medical Service) and we are also helping Brewarrina with lab testing.”
Sunita says NSW Health Pathology has provided a great network of mentors and supportive managers since she arrived in Walgett.
“In six months, I never expected to grow so much and I should give credit to Ben Alchin (Senior Operations Manager for Western NSW and Far West) for linking me with so many great people in the organisation who have helped me.”

Sunita’s advice to someone considering a tree change?
“They shouldn’t overthink it – just take the leap! Walgett is a long way from Sydney, but I do not regret one day that I made this decision. I am very grateful to be working here, because I love it here.”
Incentives to move to regional NSW
Hannah Beveridge is NSW Health Pathology’s Regional Talent Acquisition Specialist and says she loves hearing about staff who have had a successful career change into the regions.
“Sunita was able to take advantage of NSW Health’s Rural Health Workforce Incentive Scheme (RWIS) which offers financial bonuses for health staff and new employees taking up jobs in regional parts of the state,” Hannah said.
“It’s designed to attract and retain staff to regional, rural and remote NSW. Our ‘hard to fill’ positions and ‘critical vacancies’ across these locations are incentivised via a fortnightly allowance, which is worth between $10,000 and $5,000 per annum depending on the location, pro-rata for part timers.”

Hannah says one of the biggest challenges in attracting new employees to rural and regional areas is the perception that you need to live and work in a bigger metro area to grow and further your career.
“Sunita’s story is exactly what it’s all about! Her passion to help her community ignites excitement and inspires others.
“Career growth, health improvements as well as the impacts she is having to the Walgett community, is a success for everyone. Keeping our regional workforce healthy means our communities have access to local healthcare and timely results.”
Interested in a job in rural or regional NSW?
Find your next career move and all our eligible RWIS positions here!