At NSW Health Pathology (NSWHP), we manage the largest accredited Point of Care Testing (PoCT) service in the world.
This vital service has been growing since the day we went live in Narromine ten years ago, with over 1100 PoCT devices now in 190 health services across NSW.
PoCT uses mobile devices to analyse pathology samples, like blood and saliva, and provide on-the-spot results at a patient’s hospital bedside or in the community. We help to make sure that patients can get quality, reliable pathology tests, at the time they need them the most.
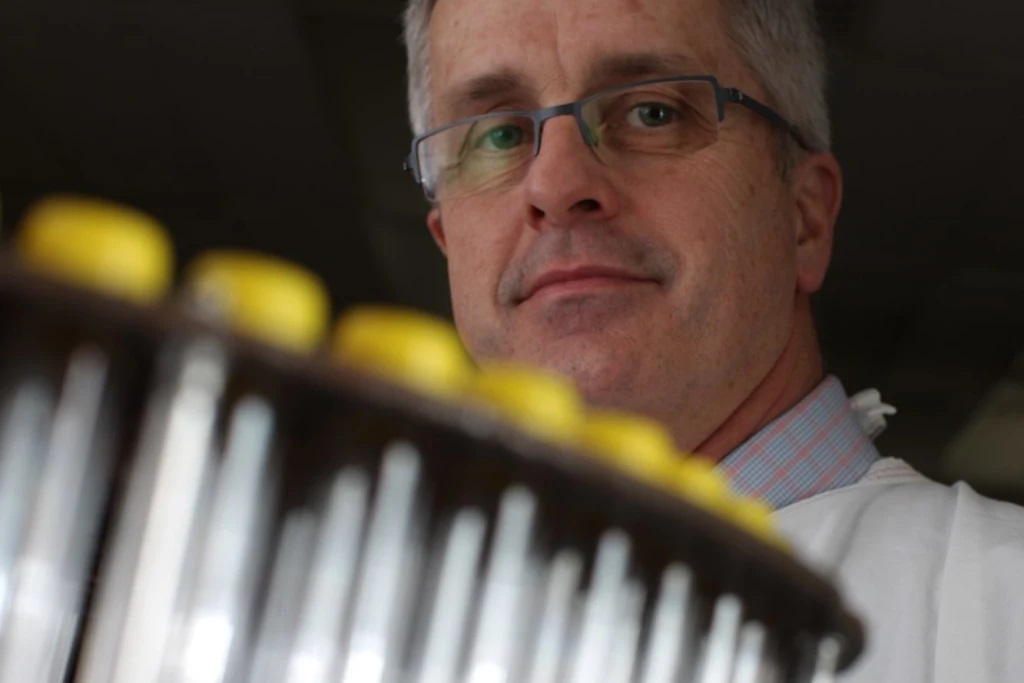
To celebrate the 10-year anniversary of PoCT and reflect on just how much the service has evolved, we caught up with a member of the original PoCT team who launched our Narromine service in 2013, Gayle Warnock, Acting Operations Manager PoCT.
What did the PoCT service look like when you launched the service at Narromine in October 2013?
Prior to 2013 when NSWHP began rolling out our PoCT network, local point of care testing was disjointed. There weren’t enough services to cover the growing demand, particularly in our rural and regional areas.
How has the PoCT service changed over 10 years?
Our service has been expanding since day one and it is amazing to reflect on what has been achieved.
We’ve added devices in more rural and remote hospitals to ensure more patients in NSW can access urgent and sometimes lifesaving pathology services.
We have worked with our NSW Health colleagues to connect existing PoCT devices that were in regular use in hospitals and clinics to electronic medical records (eMRs) and quality management systems, helping us to provide truly connected care.
We’ve continued to add new and higher-quality devices to improve our services as new technology and more point of care pathology tests became available.
Our POCT service has matured so much over the past 10 years. We have a comprehensive governance system, world leading Quality Control (QC) and Quality Assurance Plan (QAP) management tools and have developed simpler and more accessible training systems to support our health care providers and clinical teams.
We are even now branching out into AI systems and a stronger IT infrastructure to provide better insights into our PoCT service. PoCT is not just pathology! It’s a combination of technology, people and data management, melding together to shape what NSW Health and our patients and communities need now, and into the future.
What does the growth in PoCT testing mean for clinicians and patients in regional and rural communities?
The availability of PoCT can be lifesaving for people in rural and remote communities. In its most extreme examples, it provides vital emergency and primary health services like the Toll Ambulance Rescue Helicopter Service and Royal Flying Doctor Service (RFDS) with access to critical pathology results that give seriously injured and unwell patents the best chance at survival.
On a day-to-day level, local PoCT services help people to stay in their homes and communities and avoid unnecessary travel and hospital admissions. It’s so much better to be near friends and family when you’re unwell, rather than need to be transferred hundreds of kilometres from home for care.
In more metropolitan areas, PoCT also helps to break down barriers for people with challenges accessing healthcare. Those who don’t have English as a first language, who struggle with transport, isolation, or mental health issues. Having a result straight away when seeing their specialist or clinic can help provide the best care to everyone accessing NSW Health services.
What do you love most about working in the PoCT space?
I love the problem solving! There is never a dull day and I get to work with so many diverse groups both within pathology and in the clinical space. We have so many opportunities to develop systems that really contribute to patient care, to pathology and even into the growth of PoCT nationally as our peers in other states develop their own systems.
What is your vision for PoCT?
My vision is for PoCT to be a fully connected clinical resource. To support our health care colleagues, connect into clinical decision tools and patient management systems and maintain a laboratory quality standard of results.
There are so many new PoCT options available now as technology allows for smaller and smaller systems, new diagnostic markers are being found and everyone wants an immediate answer.
I want to see NSW Health Pathology as the leading voice on PoCT. To see us lead the way with validated high-quality systems that provide meaningful results to people, no matter where they are in NSW.
We are committed to developing and improving our PoCT service and can’t wait to watch it continue to grow over the next 10 years. Learn more about the service here.